A “Mountain Model” to support the public sector scale-up of health innovations
Thomas Feeny (Senior Program Director, Results for Development), Nelson Gitonga (CEO, Insight Health Advisors) and Richard Kohl (Strategy & Scale)
The scaling up of promising health innovations in Low- and Middle-Income countries (LMICs) is becoming an increasingly important area of interest for actors seeking to build efficient, resilient and adaptive health systems. The challenges of meeting the health targets set out in the 2030 Sustainable Development Goals are significant — even for those countries with mature and well-resourced health systems — and this is generating increased interest among many governments in exploring how health innovations might help to accelerate their progress.
In 2020, as the COVID-19 pandemic was spreading around the world, a team from Results for Development and Insight Health Advisors in Kenya undertook a comprehensive piece of consultative research exploring demand by public sector actors at all levels (national and sub-national) for innovative policies, products, services and/or ways of working that are designed to improve population health outcomes. Using Kenya as a case study, the report surfaced a range of interconnected factors that were influencing public sector demand for, and scaling of, health innovations, as shown in the figure below:
Each of these factors is discussed in more detail in the full report.
Designing a model to enhance public sector scaling
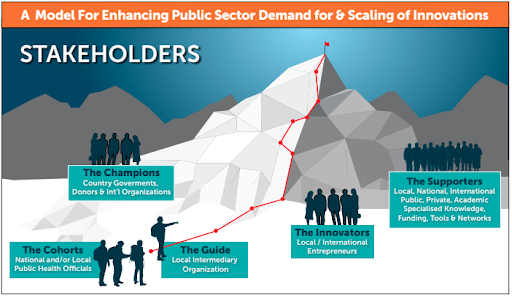
The influencing factors noted above provided a strong base of evidence that then helped to inform the collaborative design of a six-stage model that uses the metaphor of climbing a mountain to communicate the different kinds of support and intervention required at key points along the demand and scaling journey. This “Mountain Model” has the following features:
The model describes a locally-facilitated process that can respond to the challenges and opportunities surfaced through this research. Its primary goal is to provide support to LMIC national and local governments in scaling innovations that are aligned with their health priorities. This point cannot be overemphasized — it is not prescriptive. In fact, the only structure it has is a set of stages, relevant stakeholders and decision points surfaced from this research that will help to guide the overall process and ensure an efficient use of everyone’s time.
The Mountain model is designed to be demand driven as far as possible in terms of (a) meeting the needs and priorities explicitly articulated by participating public sectors actors as they work through what their demand looks like, and (b) then what assistance they would like in identifying, assessing, adopting and scaling innovations to meet those needs.
While created and tested in the context of health, the Mountain Model does not carry any bias towards particular subsectors or issues, nor will it promote or prioritize the specific innovations or interests of any international agency where these do not align with those of the country government.
The long-term, overarching goal of this model at every stage is to identify and lay the foundations for a sustainable, locally-owned process for demand and scaling, ideally through institutionalization of the associated roles and responsibilities within the public sector and its partners as appropriate
Importantly, the model was also created in line with the following design principles that government actors at all levels of the health system consistently emphasized in our consultation:
Treat demand and scaling as points along the continuum of an innovation’s journey, rather than as issues that can be addressed or enhanced in isolation
Design to the incentives (actual and potential, professional and personal) of different actors
Ensure local actors lead in determining goals, pace and direction, using Human Centered Design approaches to co-create metrics and milestones to capture engagement and sustainable capacity (rather than only those associated with the innovations being scaled)
Facilitate flexible access to different kinds of support (especially from local actors) as needs emerge, rather than one-off training / capacity-building initiatives
The Mountain Model Stakeholders
Key to this process is establishing the following five stakeholder groups (see Figure 2 below), whose expertise and resourcing will be mobilized in a demand-driven way to help address barriers as and when they emerge:
THE CHAMPIONS — Country/county governments, innovation funders and international agencies who are interested in providing overarching resources for activities to enhance public sector demand and scaling of innovation in a particular context / sector.
THE COHORT — a discrete group of national and/or local public health officials who share a willingness and ability to embark on a process of improving their uptake and scaling of health innovations.
THE GUIDE — a local intermediary organization with deep contextual knowledge and cross-cutting networks, who will listen, learn, connect and support the Cohort to different resources and actors at key points along the scaling journey to help overcome barriers. In this way, the Guide performs the critical long-term ‘hand-holding’ of government actors as they encounter inevitable challenges in ascending the mountain.
THE INNOVATORS — a pool of local, national and international entrepreneurs with solutions that can be matched, adapted and mobilized to meet the specific innovation demands of governments, as and when this demand is articulated.
THE SUPPORTERS — a pool of diverse public, private and academic actors from local, national and international contexts who can be mobilized at different points in the scaling journey to provide specialized knowledge, technical expertise, funding tools and/or networks to the Cohort based on the challenges they face.
A Six-Stage Journey through Demand and Scaling
Six broad stages were then identified that each Cohort will typically need to work through in order to make sustainable progress in sourcing and scaling innovations to meet their needs. Importantly, this process will be demand-led rather than imposed or prescriptive, and the Guide will be the key to ensuring successful mobilization of actors and resources to help address whatever challenges emerge along the way.
STAGE ONE – Articulate Demand. A key finding of our research was that while most LMICs have well-articulated policy goals and objectives, these are often not translated into a sufficiently granular level to provide new or existing innovations with obvious entry points to contribute to those goals. We expect that targeted technical assistance will be a key part of the solution here, working closely with national and local health officials to look at key gaps and inefficiencies hindering the achievement of policy goals and priorities and translating these into specific innovation entry points. Understanding current incentives (and disincentives) of different actors within the public system will also help to identify potential advocates and critics that will need to be navigated along the way.
STAGE TWO – Scan, Assess and Select Innovations. Thousands of innovations in health already exist. Though some of our interviews indicated that more needs to be done to ensure that there is a critical mass of health innovations ready for scaling, the focus of this second stage will be on helping government actors efficiently scan what it available, assess the pros and cons of different solutions and then make decisions around which they want to adapt/adopt going forward. This will require working in partnership with innovators and supporting institutions to (a) ensure that the necessary cost, impact and adoption information is available and comparable; (b) ensure they are able to clearly explain how their innovations work and how their impact is aligned with goals of concern to policymakers; and (c) articulate the potential of their innovation to accommodate contextual modification and adaptation. Subject to need / opportunity, a national or sub-national institution(s) may be engaged to lead the collection, assessment and curation of health innovations, serving as a neutral broker and convener as necessary.
STAGE THREE – Identify the Scaling Pathway. Our research suggests that there are three broad pathways for innovations to reach sustainable impact at scale through the public sector: (1) Approval and Accreditation; (2) Purchasing, Procurement and Public-Private Partnerships; and (3) Adoption and Integration. Based on an understanding of the problem being targeted, the specific demand articulated by the Cohort and the nature of the innovations that have been assessed as potential solutions, the Guide will work with the Cohort and other Supporters as necessary to map out the most cost-effective route to scale within their resource constrained environment. This will also likely involve assessing barriers / enablers associated with political will and identifying ways to create more enabling budgeting, procurement and regulation processes at different levels of government.
STAGE FOUR – Attract / Reallocate Scaling Resources. LMIC governments have limited discretionary expenditure or resources allocated to supporting innovation, at least within the health sector, and this is even more true of countries that remain more donor dependent than Kenya. We expect this stage to be especially challenging, requiring the Cohort to undertake a range of activities with the assistance of Supporters. This will likely include internal advocacy, political negotiation and influencing to attract or secure the reallocation of the resources needed. This will very likely be an ongoing process as resourcing requirements may fluctuate and once-committed resources may be reassigned as political priorities change. However, it seems that an initial ‘carrot’ of catalytic, matching funding from external donors (to cover initial innovator engagement and associated change management processes to support uptake) could be helpful in unlocking additional resources to support ongoing operating costs. Working with the Cohort to mandate responsibilities associated with the sourcing and uptake of innovations to new or redefined positions within government teams could also be effective.
STAGE FIVE – Implement, Learn and Iterate Scaling. This is a long and difficult process, yet it is ironically the implementation phase that often attracts the least attention and planning. In fact, this stage is fraught with pitfalls including the need to adapt the innovation to align with changing systems structures and processes, often on an ongoing basis. This is accompanied by a need to strengthen or modify the wider system to support scaling of the innovation. Critical in this stage is the need to continue the adaptive learning approach and supporting data collection tools from the previous stages. Monitoring is also essential to know whether the innovation is having the expected impact, and whether iterative changes in direction or implementation might be needed in order to improve progress along the scaling pathway. Generating this kind of data and convening actors for regular review and discussion is vital to the broader demonstration of impact, which in turn helps to establish and sustain credibility, ownership, demand, resourcing and political backing.
STAGE SIX – Institutionalize. The final stage of the Mountain model is actually one for which the foundations will have been laid throughout the entire process. By ‘institutionalize’ we are here referring to the capacity of the public sector actors (or other local institutions as appropriate) to independently implement the different stages of the Mountain model successfully such that demand and scaling responsibilities are integrated / mandated within existing roles and partnerships (or in new institutions). Following each stage of the Mountain model, participants will come together in a Learning Basecamp to discuss — among other things — what it would take for that stage to be locally-led and implemented on a sustainable basis. This final stage will then bring all of this together to understand what a sustainable, end-to-end version of the Mountain model might look like, who it would involve and how it would be resourced. It is impossible to say for certain how long it may take Cohorts to work through these different stages and reach the ‘Summit’ point. However, we are committed to using the Mountain model as a vehicle for empirical learning by introducing regular ‘Learning Basecamps’ during or after each of the five stages to help all of the associated stakeholders come together to reflect and exchange insights on their experience. This learning will also be used to help drive innovation and scale-enabling changes in the wider environment, targeting in particular existing institutions or departments with roles that support cross-governmental learning and support.
Milestones and Metrics of Success
In a context where there are few successful case studies to learn from, it will be important to measure the relative effectiveness of the Mountain Model against a different set of metrics to those normally associated with innovation scaling (which tend to quantify success purely in terms of people reached or impacted by the solution). Enhancing public sector demand for, and scaling of, innovation is very much a change management process, and will likely require indicators that are focused on levels of engagement and sustainability. The table below provides an early indication of what these milestones and metrics of success for the Mountain model might look like, recognizing that these will ultimately be decided in collaboration with the key stakeholder groups in the Orientation session noted above.
Testing and scaling the Mountain Model approach
Following development of the Mountain Model, approval from the Kenyan Council of Governors and with additional support from Grand Challenges Canada in partnership with Global Affairs Canada, testing of the Mountain Model began in early 2022 with two cohorts from the Makueni and Kajiado county governments in Kenya. Facilitated by a team from Insight Health Advisors, these pilots are demonstrating how valuable frameworks such as the Mountain Model can be in supporting government-led demand and scale-up of health innovation. In 2022, the Global Financing Facility at the World Bank also supported testing of the first few stages of the Mountain Model with a national-level cohort of government actors from Tanzania, to great success, and in 2022 the Mountain Model was adopted as an organizing framework for the first ever ‘Public Sector Scaling Action Lab for East Africa. In 2023, Results for Development was also invited to work with the innovation team of the World Health Organization to use the Mountain Model as the basis for a global “Call to Action on Enhancing Public Sector Scale-up of Health Innovation,” which will be launched at the inaugural Global Health Innovation Forum in India.
The future is exciting! If you would like to know more about the Mountain Model, please contact Tom Feeny (tfeeny@r4d.org).